
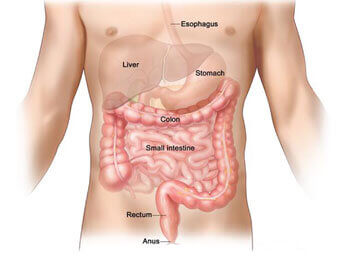
Rectal prolapse is a medical condition in which the rectum starts to push through the anus. The rectum is that last part of your large intestine, and the anus is the opening through which stool exits your body.
It’s often suspected when the problem is actually a serious case of hemorrhoids.
Rectal prolapse can range from mild to severe. Mild cases can often be treated without surgery. Severe cases may require surgery.
The symptoms of rectal prolapse tend to come on slowly. The first symptom you’ll notice is the feeling that there is a bulge at your anus. It may seem as though you are sitting on a ball.
Normal physical activity, such as walking, sitting, and exercising, may also cause part of the rectum to push through your anus. At first, it can be returned to its proper location by hand.
If rectal prolapse worsens, there could be bleeding from the inner lining of the rectum. In cases of partial or complete prolapse, you may have trouble controlling liquid or solid bowel movement and gas from your rectum.
Up to half of the people with rectal prolapse experience constipation, while others may have episodes of constipation and incontinence.
There are three types of rectal prolapse. The type is identified by the movement of the rectum:
Rectal prolapse can be caused by several medical conditions. They include:
If nerves that control the rectal and anal muscles are damaged, rectal prolapse can develop. These nerves can sometimes be damaged from:
This is the muscle that allows stool to pass from your rectum. Common reasons for this muscle to weaken are pregnancy and childbirth, or increased age.
The strain of chronic bowel movement problems can make your rectum more likely to move down from its location. Strain while having bowel movements, if done often over a period of years, can also cause rectal prolapse.
While not directly linked to rectal prolapse, some conditions may increase your risk for it, including:
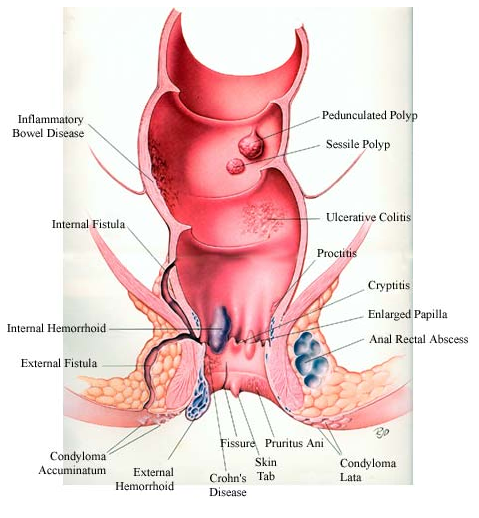
Rectal prolapse and hemorrhoids can both be uncomfortable and very painful conditions. Rectal prolapse may initially feel like a bad case of hemorrhoids, and sometimes hemorrhoids on your anus may look as though your rectum is emerging.
Rectal prolapse involves movement of the rectum itself. Hemorrhoids are actually swollen blood vessels in the walls of your rectum or anus. Hemorrhoids, though quite common in their smaller, milder form, can become painful and itchy. They can leave red blood on tissue when you wipe. Rectal prolapse can also cause bleeding sometimes.
Rectal prolapse won’t get better on its own. The degree of prolapse will increase over time. This process can take months or years, so there isn’t always a rush to make a decision.
If you’ve been diagnosed with rectal prolapse, you may choose to delay treatment if your symptoms are mild enough and your quality of life isn’t significantly hampered.
Surgery is the only way to effectively treat rectal prolapse and relieve symptoms. The surgeon can do the surgery through the abdomen or through the area around the anus.
Surgery through the abdomen is performed to pull the rectum back up and into its proper position. It can be done with a large incision and open surgery, or it can be done laparoscopically, using a few incisions and specially designed smaller surgical tools.
Preventing rectal prolapse isn’t always possible. You can reduce your risk if you maintain good intestinal health. To help avoid constipation, in particular: